Medicaid (known as TennCare in Tennessee) is a federal-state partnership program that pays for about half of long term care costs in America (excluding the costs of in-home care provided by families). Federal law sets out the limitations on assets that determine which seniors are eligible for Medicaid assistance with long term care costs. Although states do provide some regulations that interpret those provisions about assets and income limits, most of the requirements are federal.
Tennessee responded by revising the medical requirements for an individual to qualify for nursing home services effective July 2, 2012. Persons must have a score of 9 or above on the scale set out below to qualify for nursing home care.
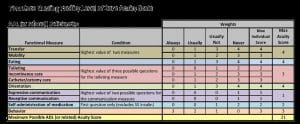
As you will see from this chart, transfer and mobility are grouped together. Transfer measures the ability to transfer to and from bed, chair or toilet without the assistance of someone else. Mobility measures the ability to walk without physical assistance from another person. The need for a wheelchair, walker, crutch or cane does not satisfy this requirement. If a person can never transfer without assistance and never walk without assistance, the highest score in this category is a 4.
Eating measures a person’s inability to place food and drink in his or her mouth. Someone who cannot prepare food, set up a tray or cut up food gets no points here as long as he or she can transfer the food or drink from plate to mouth.
Toileting, incontinence care and catheter care/ostomy care are grouped together. Again, it is the need for physical assistance from another person that is measured. The highest score for someone who always needs care in one or all three of these areas is a 3.
The remaining categories deal more with dementia and less with physical restrictions. For someone who is disoriented to people or place (fails to remember his or her own name or family members or fails to remember residence in a nursing home or wherever) the highest score is 4.
A person who is never able to communicate basic needs or wants can score 1 point. If he or she can never follow simple instructions without continual intervention from someone else, another point. If such people can sometimes communicate or follow instructions, no points are awarded whatever.
Medication administration measures inability to place medication in one’s mouth and swallow it. Needing assistance with reminders to take medicine, encouragement to take it, reading labels, opening bottles, handing medicine to the person and reassurance as to the correct dose don’t count at all in determining whether a person scores anything on this measure. The highest score for someone who always needs help putting the medicine in his or her mouth and swallowing is a 2.
Behavior measures the need for persistent intervention by someone else because of a pattern of dementia-related behavior problems, such as wandering, disrobing, or aggressive physical behavior. The highest score for someone who always needs intervention is a 3.
Adding up the possible scores shows that someone who is physically mobile but demented is going to have advanced dementia to qualify for nursing home care.
Documentation is an important issue. The family of someone who is being cared for at home may have difficulty in coming up with documentation to support deficiencies in the ability to perform some of these activities.
Fortunately, there is some wiggle room if the applicant’s needs can’t be safely and appropriately met in the community.
On the whole, however, lawyers in Tennessee specializing in Elder Law are seeing people who formerly would have qualified for nursing home care being denied on the basis of this new scoring system.